Information
The individual sensitivity of a person’s hearing, the hearing threshold, is the quietest sound a person can hear. The measurement of this threshold is called audiometry. There are different methods to locate the hearing damage and determine the nearing capacity.
Even children with a normal hearing capacity first have to “learn” to hear. What is known as the auditory system is developed during the first year of life. This means that the brain only gradually links and interprets sounds with certain auditory impressions. The hearing threshold for sound for a newborn with healthy hearing is around 80 dB HL and goes down to 0-20 dB HL during the first year of life. In infants and toddlers, the threshold is determined in a “free field” environment. This test takes place in a sound-insulated room. Usually, the child sits on the parent’s lap or in the pram or pushchair during the test. Acoustic stimuli with different frequencies and volumes are played through the speakers. Based on the child’s reactions (changes in breathing, eye movements, pause movements for a moment, e.g. sucking on a dummy, startle response, etc. of possibly locating the source of the sound in older children), the child’s hearing response to the varying volumes of the different frequencies is observed.
Since every child reacts differently to acoustic stimuli, the audiologist needs a lot of experience and routine when judging evoked-response audiometry and hearing reactions. The evoked-response audiometry can also be performed with hearing aids and thereby allows for an evaluation of the hearing success, a control of the settings and comparison between different hearing aids and/or settings.
If children are 2-3 years or older, the hearing threshold can usually be determined by what they tell you. This process is done playfully. The child is instructed to do a fun activity when he or she hears a tone or sound. At this point, tone audiometry is measured through speakers. When children are a little older and have no issues performing the activity, the measurement is performed separately on each side with headphones. The following pictures demonstrate examples of tone audiograms which were recorded on the headphones; in each case the right ear is shown. The upper, dashed line marks the measurements via bone conduction. With the aid of a special hearing device, the specific tone can be transferred into the inner ear by vibrations of the cranium bone. The lower line shows the measurement via aerotympanal conduction, i.e. with normal headphones. Since the tone has to “pass” the middle ear before it can reach the inner ear, this curve can never be better than the bone conduction.
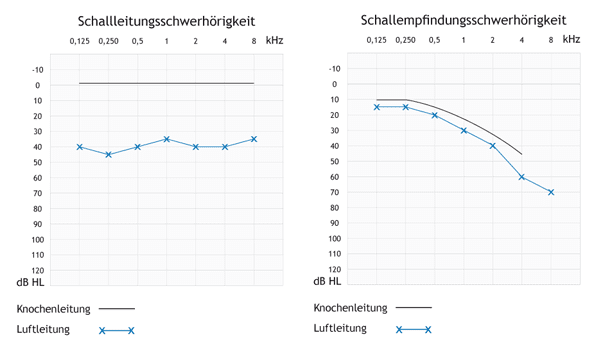
The audiogram in the top left-hand corner shows the audiogram of a person with normal binaural hearing. The aerotympanal conduction and bone conduction should be in a range of 0-20 dB HL and should differ from each other by no more than 15 dB.
In the second audiogram in the top right, you can see purely conductive hearing loss. The bone conduction shows normal results across the entire frequency range. Nevertheless, the aerotympanal conduction is shifted down 35-45 dB in comparison to the bone conduction. This might be due to a bruise in the middle ear, which affects the acoustic sound from being transferred to the inner ear.
The audiogram at the bottom shows sensorineural hearing loss. Aerotympanal conduction and bone conduction are parallel and very close to each other. The demonstrated hearing loss is more distinctive in high tones. This trend can be observed if the inner ear is damaged.
Objective audiometry (e.g. ABR or BERA) allows the “actual” hearing threshold to be measured immediately after birth. This threshold will normally be between 0 to 20 dB HL and therefore cannot be initially equated with the reaction threshold. The objective audiometry is used in the scope of determining the hearing threshold. With babies and little children, it is usually conducted when they are asleep because movements in the muscles can affect the quality of the results and hence prohibit an accurate assessment of the child’s ability to hear. In order to ease falling asleep, a sedative is given. Measurements under anesthetic are performed in rare cases and under special circumstances.
In order to measure the BERA, three to four single-use electrodes are affixed to the scalp. During the measurement, acoustic stimuli (with frequencies between about 2 and 4 kHz) are delivered to the ear via headphones. Voltage changes can be captured on the scalp through the electrodes. This way, it can be decided whether the acoustic stimuli are processed at a certain volume and are transferred through the auditory system to the brain stem. The so-called “potential”, meaning the response threshold of the hearing impression in the EEG, is subtly different for each child. Additionally, it is dependent on measurement conditions. An important factor is the sleep of the child. Restlessness, movements, snoring and so on can affect the quality of the measuring results. As with the reaction audiometry, the examiner needs routine and experience to accurately assess the derived potentials. Since the measured curves have to be visually evaluated, the BERA is sometimes known as the semi-objective test procedure.
Methods which allow for a more detailed determination of the frequencies within the audiogram are now also available. The “Notched-Noise-BERA” (NN-BERA) is the most commonly used. Whether a NN-BERA can be performed depends on whether or not the child sleeps long enough, since the aim is a measurement/confirmation of the hearing threshold. Hence, a second examination might be necessary.
In order to check and locate the hearing impairment, audiologists use the measurements of optoacoustic emissions (OEAs). However, these only allow for the efficiency of the inner ear, more precisely of the outer sensory hair cells, to be assessed, if they are verifiable. If it is not possible to measure OAEs, there might be a variety of reasons and it does not necessarily mean that the child has hearing loss. In most cases, there is only a problem in the ventilation dues and sometimes it is due to unfavorable measuring conditions (e.g. restlessness or noise made by the child, ambient noise, measuring head which was clogged with earwax). Furthermore, even people with normal peripheral hearing capacity sometimes do not have sufficient optoacoustic emissions.
When performing a diagnostic measurement of optoacoustic emissions, the replicability of the answers is stated as a percentage. Often, this is misinterpreted as a percentage of hearing impairment. Generally speaking, a hearing impairment cannot be classified this way since its results differ within the frequency ranges of human hearing. The possible curves of the audiogram as well as the extent of the hearing loss have to be specifically assessed depending on the categorization.
Hearing loss is divided into three categories:
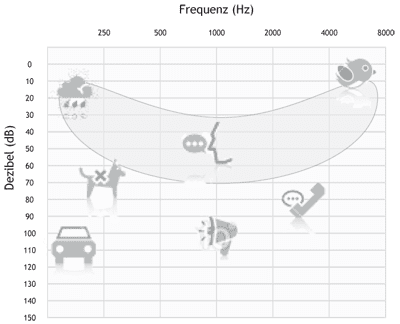
The scale at the bottom shows the high tones on the right of 1000 Hz, the low tones on the left of 1000 Hz. The red area is defined as the speech banana. It demonstrates the areas in which different letters are recognized. The pictures show the sounds your child cannot hear if suffering from the specific hearing loss.